Telemedicine Innovations 2026 are redefining how patients access care, how clinicians monitor chronic conditions, and how health systems allocate scarce resources across communities. As adoption expands, remote patient monitoring is becoming a core component of proactive care, enabling early detection, personalized intervention, and more predictable outcomes for diverse patient populations. This evolution is supported by interoperable devices, secure data exchange, and AI-driven insights that connect clinicians, patients, and caregivers wherever care is needed. As a result, care teams can coordinate more effectively, reduce delays, and sustain high safety and privacy standards across increasingly virtual care workflows. Taken together, these dynamic factors are reshaping the delivery of care into a more connected, patient-centered, and outcome-driven system.
Beyond the explicit label of telemedicine, the current momentum reflects a broader shift in telehealth, digital health ecosystems, and integrated care platforms. This LSI-inspired approach emphasizes virtual care concepts, patient empowerment, and data-informed decision making that spans primary, specialty, and urgent care. Organizations are building interoperable workflows, scalable remote monitoring capabilities, and security-first architectures to support continuous engagement. In short, the 2026 landscape favors an integrated model of care where connectivity, analytics, and human support combine to extend reach, improve outcomes, and elevate patient experience.
Telemedicine Innovations 2026: A Catalyst for Healthcare Digital Transformation and Access
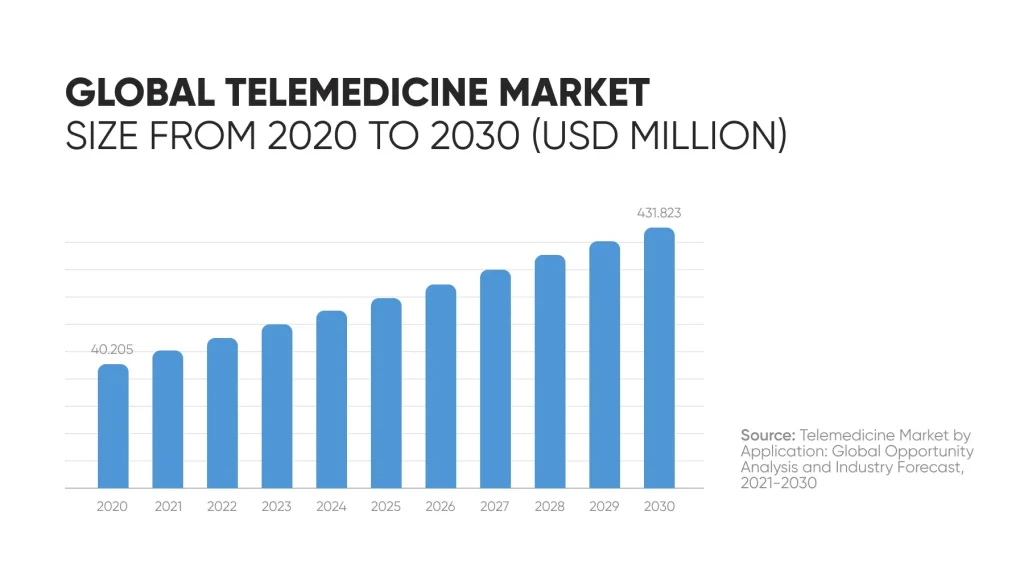
Telemedicine Innovations 2026 are reshaping how patients access care and how health systems allocate resources, marking a pivotal moment in healthcare digital transformation. This era embraces telemedicine 2026 trends that blend advanced connectivity, data analytics, and patient-centric design to extend care beyond traditional clinic walls. By prioritizing remote care technology that supports real-time decision making, organizations can deliver safer, more efficient services while maintaining a strong focus on privacy and quality.
As access expands to rural communities and underserved urban areas, patients experience more convenient, timely encounters with clinicians who can monitor conditions remotely and adjust plans proactively. The convergence of telemedicine with remote patient monitoring and wearables creates a continuous data stream that informs every encounter, turning episodic visits into ongoing care journeys. This shift underpins a broader push toward healthcare digital transformation, where digital tools are embedded into routine workflows to improve outcomes without sacrificing safety or equity.
Remote Patient Monitoring and Wearables: The Backbone of Modern Telehealth
Remote patient monitoring has evolved from a niche capability into a foundational element of comprehensive care. Modern devices continuously track vital signs, glucose levels, activity, and respiratory metrics, feeding data to clinicians in near real time. When deviations occur, automated alerts prompt timely interventions, helping to prevent crises and support chronic disease management through telemedicine sessions that are more informed and focused.
Wearables complement traditional monitors by enriching longitudinal health data that can be integrated into electronic health records. This seamless data fusion enables clinicians to see trends over time and tailor treatment plans within virtual care encounters. The result is a more proactive approach to health management, faster response times, and a stronger alignment between remote care technology and patient outcomes—a central theme in telemedicine 2026 trends.
Virtual Care Advancements Expanding Access Across Specialties
Virtual care advancements are broadening access across primary care, specialty clinics, and hospital services. By embedding virtual visits into standard workflows, healthcare providers can deliver timely assessments and follow-ups, even when in-person visits aren’t feasible. This expansion supports a more responsive care model, enabling urgent evaluations, chronic disease management, and mental health services to be delivered through secure, user-friendly platforms.
Patient experience is enhanced when platforms offer multi-disciplinary collaboration, real-time messaging, and robust educational resources. Virtual care rounds and family-centered approaches connect patients with care teams regardless of location, empowering people to participate actively in their health journey. As users report higher satisfaction and adherence to care plans, health systems see the tangible benefits of combining convenient remote access with high-quality, evidence-based care.
Interoperability and Secure Infrastructure for Scalable Remote Care
A solid interoperability foundation is essential for scaling telemedicine. Standards such as FHIR enable seamless data exchange across devices, platforms, and health systems, reducing duplicate work and enhancing accuracy. Cloud-based infrastructure provides scalable, compliant resources that can adapt to growing demand while maintaining strong security controls. This infrastructural backbone is a key enabler of healthcare digital transformation, ensuring that virtual visits integrate smoothly with broader care pathways.
Beyond technical interoperability, robust privacy and security controls are non-negotiable. Regulatory requirements demand encryption, strong authentication, and regular audits to protect sensitive health information. When aligned with staff training and governance policies, these measures help sustain patient trust and ensure that remote care technology remains a reliable option within both virtual and in-person care models.
AI-Driven Efficiency and Clinical Decision Support in Telemedicine
Artificial intelligence is elevating telemedicine from a simple video visit to a comprehensive care experience. Natural language processing captures and structures clinical conversations, enabling faster documentation and freeing clinicians to focus on patient interaction. Predictive analytics identify individuals at risk of hospitalization, allowing proactive outreach during telemedicine sessions and remote monitoring.
Decision support systems deliver evidence-based recommendations that align with patient preferences and local guidelines, while workflow automation reduces administrative burdens such as prior authorizations and documentation. Together, these capabilities increase clinician efficiency and enhance the quality of care delivered in both remote and in-person settings, reinforcing telemedicine as a robust component of modern healthcare delivery.
Practical Steps for Health Systems to Implement Telemedicine Innovations 2026
A pragmatic roadmap for success emphasizes interoperability, data governance, and scalable cloud platforms. Health systems should prioritize user-friendly patient portals, secure messaging, and streamlined previsit workflows to support the patient experience within telemedicine innovations 2026. By aligning technology choices with clinical guidelines and quality metrics, organizations can realize measurable improvements in access, safety, and outcomes.
Beyond technology, effective implementation requires governance, training, and stakeholder collaboration. Organizations should involve clinicians, IT staff, and patients in design and testing, monitor utilization analytics, and iterate processes to close gaps in digital literacy and equitable access. A patient-centered approach—coupled with continuous improvement—ensures telemedicine remains a trusted, high-quality option that supports the broader digital transformation of healthcare.
Frequently Asked Questions
What are Telemedicine Innovations 2026 and how do they redefine access to care?
Telemedicine Innovations 2026 represents the integration of telehealth with advanced remote care technology, 5G-enabled real-time video, edge computing, and AI-powered tools, making virtual care a core component of everyday healthcare. It expands access beyond pop-up clinics by embedding virtual visits into standard workflows, benefiting rural and underserved populations and supporting healthcare digital transformation.
How do remote patient monitoring and wearables fit into Telemedicine Innovations 2026?
Remote patient monitoring (RPM) uses wearable sensors to capture vital signs in near real time; clinicians receive alerts when thresholds are crossed, enabling proactive care and better chronic disease management. Data from wearables flows into electronic health records, creating a longitudinal health view that enriches telemedicine consultations.
Why are interoperability standards essential for Telemedicine Innovations 2026?
Standards like FHIR enable seamless data exchange across devices and platforms, supporting a unified patient record during virtual visits. Interoperability reduces duplicate data entry, supports cloud-based infrastructure, and underpins a secure, scalable healthcare digital transformation.
What practical steps can health systems take to implement remote care technology in Telemedicine Innovations 2026?
Invest in scalable cloud platforms, define data governance, and build modular IT architectures; integrate patient portals, telemedicine workflows, and remote monitoring programs; train staff and establish clear privacy and security policies to maintain quality, safety, and patient trust.
How do virtual care advancements influence patient experience in Telemedicine Innovations 2026?
Virtual care models deliver multidisciplinary teams, virtual rounds, and patient-centered communications across devices; patients benefit from rapid access, clear information, and follow-up; user-friendly interfaces and education resources boost engagement and satisfaction.
What challenges and opportunities do providers face with Telemedicine Innovations 2026, including privacy and security?
Key challenges include integrating remote visits into existing workflows, navigating evolving reimbursement, and addressing digital literacy and equity. Opportunities include scalable care delivery, AI-assisted triage, and improved outcomes, but require strong encryption, authentication, access controls, and ongoing staff training.
| Key Point | Summary |
|---|---|
| Overview | Telemedicine Innovations 2026 redefine access, monitoring, and resource allocation, advancing from necessity-driven adoption to sustainable remote care. |
| Key drivers | 5G connectivity, edge computing, AI triage and decision support, automated documentation, and wearables enabling continuous data streams. |
| Trends and access | Mainstreaming across primary, specialty, and hospital settings with flexible access and evolving reimbursement recognizing telemedicine as equivalent to in-person care when appropriate. |
| Remote monitoring | Home monitoring devices track vital signs and activity, generating alerts and a longitudinal health record integrated into EHRs. |
| Patient engagement | User-friendly interfaces, platforms enabling chat, asynchronous messaging, reminders, and education to support adherence and collaboration. |
| AI and efficiency | NLP transcribes conversations, predictive analytics flag risk, decision support provides evidence-based recommendations, and automation reduces admin tasks. |
| Virtual care experience | Multidisciplinary teams, virtual rounds, and family-centered care across devices and locations; emphasis on clear communication and follow-up. |
| Interoperability | FHIR standards, cloud infrastructure, modular IT architectures; reduces duplicate data entry and enables unified records. |
| Regulatory/privacy | Encryption, authentication, access controls, audits; ongoing staff training and compliance to safeguard privacy. |
| Evidence and outcomes | Remote monitoring improves chronic disease control, reduces ED visits and hospitalizations, and improves care coordination. |
| Challenges and opportunities | Workflow integration, reimbursement navigation, training; opportunities for scalable, equitable care and continuous improvement. |
| Future steps | Prioritize user-friendly portals, data governance, scalable cloud platforms, and alignment with clinical guidelines and quality metrics. |
Summary
Telemedicine Innovations 2026 represents more than a technology upgrade; it marks a fundamental shift in how care is designed, delivered, and experienced. By prioritizing patient engagement, interoperability, and robust data governance, health systems can deliver safer, more efficient, and more equitable remote care. The ongoing maturation of connectivity, devices, and AI supports proactive management of chronic disease, improves access for rural and underserved populations, and enhances care coordination across settings. Realizing these benefits requires thoughtful implementation: integrating telemedicine into standard workflows, investing in workforce training, aligning policies and reimbursement, and maintaining privacy and security at every step. As stakeholders collaborate across clinical, IT, and patient communities, Telemedicine Innovations 2026 can drive healthier communities with improved outcomes and patient empowerment, anchored in quality and trust.